AI in Healthcare: An evening with Dr. Geetha Manjunath
On Friday, September 19, we had an insightful session by Dr. Geetha Manjunath, the Founder, CEO and CTO of NIRAMAI Health Analytix. She spoke about AI in healthcare and the innovations her company has pioneered. Niramai has developed a breakthrough artificial-intelligence-based test for detecting early-stage breast cancer in a non-invasive radiation-free manner.
About Dr Geetha Manjunath
Dr Geetha Manjunath is a Computer Scientist with a PhD from Indian Institute of Science and management education from Kellogg’s, Chicago. She has over 25 years of experience in IT innovation and has led multiple AI projects at Xerox Research and Hewlett Packard Labs. Before starting Niramai, Dr Manjunath was the Lab Director for Data Analytics Research at Xerox. She has received international and national recognition for her innovations and entrepreneurial work, including CSI Gold Medal, BIRAC WinER Award 2018. Dr Manjunath is also on the Forbes List of Top 20 Self-Made Women 2020. She was awarded the Accenture Vahini Innovator of the Year Award by Economic Times and Women Entrepreneur of the Year 2020 by BioSpectrum India. Dr Manjunath is coauthor of the book "Moving to the Cloud" and holds 50+ US patents.
Why she entered this sector
Dr Manjunath had a successful career in HP Labs, Xerox and IISc. Why did she embark on a start up? Two close family members had contracted breast cancer and died within a year. Dr Manjunath felt the pain from close quarters and wanted to do something about it. She began to explore how to apply AI in healthcare. And that is the essence of a startup: feeling strongly about a problem and then trying to solve it.
What can AI in healthcare do?
Better patient experience: AI can be used to coordinate meetings with different doctors, treat patients as customers and value their time and increase the ease with which they can navigate the system. This is just like traveller experience in airlines.
Improved outcomes: A good example is personalized medicine. The body is a very complex system. Different people respond to the same dug in different ways. AI is being used for developing personalized medicine and medications, e.g. chemotherapy dosages. AI is also enabling robotic surgery and remote surgery.
Reduced costs: Optimize the use of resources. For example, AI can ensure that the ICU is used only for high priority patients.
Reduced misdiagnosis/overdiagnosis: AI can lead to less False Positives and False Negatives. A false positive is a false alarm, incorrectly indicating a condition is present when it is not. A false negative is a missed detection, incorrectly indicating a condition is absent when it is present.
There are two classes of applications in healthcare: Nonclinical (similar to other domains, e.g. patients chatting with doctors) and clinical (exclusive to medicine).
It is difficult to develop and commercialize AI applications in healthcare. There is little scope for error.
Consider entertainment one of the first sectors to use AI. Companies like Netflix have leveraged AI in a big way. Netflix’s recommendation algorithms suggest movies to us. But if we are not happy with the recommendation, we can skip and go to some other movie. (The algorithm keeps learning in the process.) So, the impact of an error is less.
Google Search, Customer care, Transportation, Education have all leveraged AI in a big way and benefited. Here too, the impact of an error is within limits.
Healthcare is pretty much the last sector where AI has penetrated due to various challenges.
There is a class imbalance. Only 0.04% of the people may be ill. Ideally, we want an equal proportion of healthy and non-healthy people.
Data availability is also a problem. In many classification situations, data is easily available. But that is not so in the case of healthcare. Consider breast cancer. There are many types of breast cancer. There are situations which resemble breast cancer but are not so.
Data collection is not easy. It can vary across countries and ethnicity.
Testing has its nuances. Regulatory approvals are needed.
Communicating the outcome to the patients can be tricky.
Integrating AI into clinical pathways is also challenging.
Data privacy is another challenge.
Despite all the challenges, AI can make a tremendous impact in healthcare. After all lives are at stake. For Dr Manjunath, a key benefit is that AI can reduce the healthcare divide. Poor countries / rural areas with limited infrastructure can benefit from the availability of AI based tools.
In urban areas, medical infrastructure is available. But the cost of treatment can be prohibitive. AI tools can make treatment more affordable. These tools can help interns and para medical staff in their day-to-day work.
Breast cancer is the leading cancer among women. There are 684,000 deaths in a year (2020 figures). There are 2.2 million new cases every year. Mortality rates exceed 50% in many developing countries. The key point to note is that breast cancer is curable provided there is early detection.
Thermanalytics
Niramai’s approach is to measure temperature variation across the chest. There is no radiation. A portable, light, small screening device is used to detect stage zero cancer much before a lump is felt. The treatment is affordable, non-contact and non-invasive. (The cost of the test is only Rs 100 per scan in rural areas and half the price for other tests in urban settings.)
Privacy is ensured as the test is done in changing rooms with curtains. The tool generates a visually interpretable image.

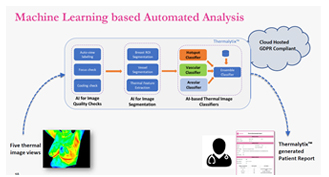
NIRAMAI uses 25 different algorithms. The model has a high degree of explainability. A hotspot classifier identifies clusters of high activity or density in each area. A vascular classifier specifically evaluates blood vessel characteristics, such as density, flow, or the presence of "hotspots" (areas of increased blood flow) in a region. Areolar classifier is based on the human areola, the pigmented area on the breast around the nipple. An areola is a small circular area with a different histology from the surrounding tissue.
The tool marks the area of lesion so that it can be checked. End users (like healthcare workers) can make mistakes. With the help of the tool, errors can be minimized.
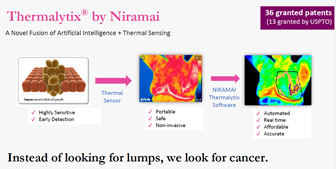
The tool has been clinically validated by several clinical studies. Extensive testing has been done to establish correlation of report findings with mammograms, ultrasound and biopsy. Hospital head-to-head testing has been used. So, the sensitivity is very high. Screening sensitivity is 100%. False positives are only 7.6%.
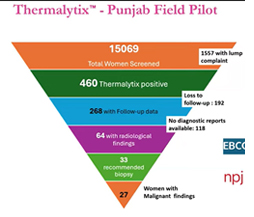
Some 300,000 + women have been screened in 25 countries (including Europe and the US) in 300+ hospitals. Since it is portable/ privacy/radiation free, the tests can be done in corporate offices. Google, American Express, Mercedes Benz, Microsoft are among the companies using it for their staff. The device is also used for screening in rural camps.
The vision is to cover every country. With the same approach, other kinds of abnormalities can also be diagnosed. NIRAMAI plans to collaborate with others.

Learning
Dr Manjunath summarized her learning:
- We must focus on real impact
- We must focus on proving the science.
- The aim of AI is not to replace doctors. Doctors plus AI will be better than doctors alone.
- Where there are not enough doctors, triaging can be used to reduce the load on the medical profession and hospitals. In Punjab using the tool, the number of women to be screened in hospitals was reduced from about 15,000 to 400.
Q&A
We must create enough scientific evidence. Any claim must be fully validated with clinical studies following ethical principles. These have been formalized as Helsinki protocols for conducting clinical trials.
Note: The Helsinki protocols refer to a set of ethical principles for medical research involving human participants. The welfare of the research subject must always take precedence over the interests of science and society. There should be fully informed consent. Research should be based on a thorough knowledge of the scientific background.
We should articulate the results depending on the audience: doctors (more technical terms can be used), marketing staff, etc.
We should talk with stakeholders as equals (i.e. not to show our superiority) and try to inspire their confidence and build trust. We should identify the trust building factors and address them in our dialogue with the medical community.
In the last 8 years, Dr Manjunath has spent little time reading technical books. She has been more focused on medical books. She has attended several medical conferences and workshops and tried to immerse herself in the domain. Dr Manjunath is in touch with leading oncologists in India, the US and Europe.
Dr Manjunath has attended workshops on interpreting mammograms, MRIs and ultrasound. She has gone deeper into different aspects of the anatomy and physiology of the breast. She has learnt that when there is a lump in the mammogram, radiologists should look for irregularity. In ultrasound we must differentiate between larger and taller.
To develop good applications in healthcare we need to combine handcrafted and deep learning features. So, Dr Manjunath’s message to techies is that it is important to keep learning about the domain.
IBM Watson created a lot of hype. After 6-7 years and $4 bn of investment, it is now seen as a failed experiment. What went wrong?
Dr Manjunath emphasised that Watson may have failed but it did showcase the potential of AI. Today with LLMs and greater computing power, learning and retraining has become much faster. And model accuracy continues to improve.
One lesson from Watson is that we should make claims only after accumulating medical evidence. We should speak and market scientific facts. We should promise less and do more.
We should not push technology with the objective of replacing existing modalities. Every imaging modality has its positives. So, technology should supplement what is going on now. Technology cannot make the final diagnosis such as the depth of the lesion. That can be made only by a competent doctor. Thermonalytics is not a substitute for biopsy. But in rural areas, technology can be a boon to many people who cannot afford to have a mammogram. In general, we should combine a mamo with thermo for the best outcomes.

The founding team consisted mostly of techies. The early days were about examining the data and crafting the right features.
Dr Manjunath and her colleagues would visit hospitals. They even took the thermal image of a person who was going for surgery the next day. They studied in depth a small group of about 120 patients consulting doctors on various aspects of each patient. Dr Manjunath refers to them as the golden set.
As they got a better hang of things and generated labelled data, Dr Manjunath’s team was also able to make out why false positives and false negatives were occurring. Once the patterns were clear, the learning was incorporated in the model to improve accuracy.
Today, there is a data science team headed by one of the founders, Shiva. Then there is an engineering team consisting of research engineers and full stack engineers. There are also product managers who define the product features. There is a regulatory team which can deal with the likes of FDA. A clinical team consisting of doctors, examines data and looks for evidence. One experienced doctor in the Philippines had data from 12,000 screenings. The team helped make sense of the data. Dr Manjunath employs interns in a big way. There are also consultants (radiologists) who work part time.

The aim is to keep false negatives close to zero. Sometimes, the disease is not detected due to specific conditions. Consider nipple discharge, a condition where fluid leaks from one or both nipples. It is a common symptom that can range from being completely normal (physiological) to being a sign of an underlying medical condition (pathological). So in case of nipple discharge, a full diagnosis is recommended in the NIRAMAI report.
AI in mammography is quite common. It is getting integrated into the picture archival systems.
Liquid biopsy is a blood test for all cancers, especially to predict the chances of recurrence.
Genetic testing is being used to identify high risk women for screening.
Radiology is probably the most happening space for AI. RSNA (Radiological Society of North America) is the largest gathering of radiologists in the world. There is a whole floor dedicated to AI showcase.
The end user is not directly looking at the AI results. There is always a human in the loop. Moreover, surveys indicate that end users do not want to be treated only by AI.
Over time, NIRAMAI has attempted to present the results in a more doctor friendly way and move the reports closer to what the doctors are used to seeing. The BI-RADS scoring system (which stands for Breast Imaging Reporting and Data System) is a standardized quality assurance tool used by radiologists to describe the findings of breast imaging tests, such as: Mammography, Breast Ultrasound and Breast MRI. Developed by the American College of Radiology (ACR), the primary goals of the BI-RADS system are to:
Standardize Reporting: Ensure that all radiologists use the same clear and consistent terminology across all facilities.
Communicate Risk: Assign a definitive category that estimates the likelihood of the finding being cancerous.
Guide Management: Provide clear recommendations for the next steps (e.g., routine screening, short-term follow-up, or biopsy).
The system uses a scale from 0 to 6, with each number corresponding to a specific assessment and follow-up plan. Zero means incomplete. 1 means negative. 2 is benign. 3 is probably benign. 4 indicates suspicious abnormality. 5 is highly suggestive of malignancy. 6 is for proven malignancy.
NIRAMAI uses BScore (Bharat Score) which is well aligned with BI RADS.
It is important to work with key influencing doctors to try out the tool and see for themselves the predictions it is making. We should also present the scientific evidence. Then doctors themselves will speak about it. Outside India, it is easier. Dr. Manjunath gave the example of an experienced oncologist in the Philippines. He is talking about the utility of the tool in different forums.
Usually, the report is signed by the doctor after reviewing the answer. So the doctor is ultimately accountable. But NIRAMAI has liability for answers generated by the tool. So there is a joint responsibility. It depends on where the error is. Suppose the tool arrives at a B Score of 5 (suggestive of malignancy) and the doctor recommends that there is no further investigation required. Then, the fault lies with the doctor and not with the tool.
